MRI Prostate Cancer Detection
Prostate Cancer Detection: What Should I know?
It is commonly thought that the PSA blood test detects prostate cancer. This is not the case. The PSA test is not specific for cancer. A higher result than normal can indicate many noncancerous prostate conditions besides cancer. Therefore, more information is needed. Commonly, urologists recommend an immediate ultrasound-guided needle biopsy (TRUS biopsy), an invasive procedure with risks of pain and infection. Why go through that before knowing if cancer is actually present or having the benefit of identifying a target in the prostate of where it might be?
The Sperling Solution
The Sperling Prostate Center provides a better way to detect prostate cancer before rushing to biopsy.
If your PSA is elevated and your MRI is normal you may not need a biopsy.
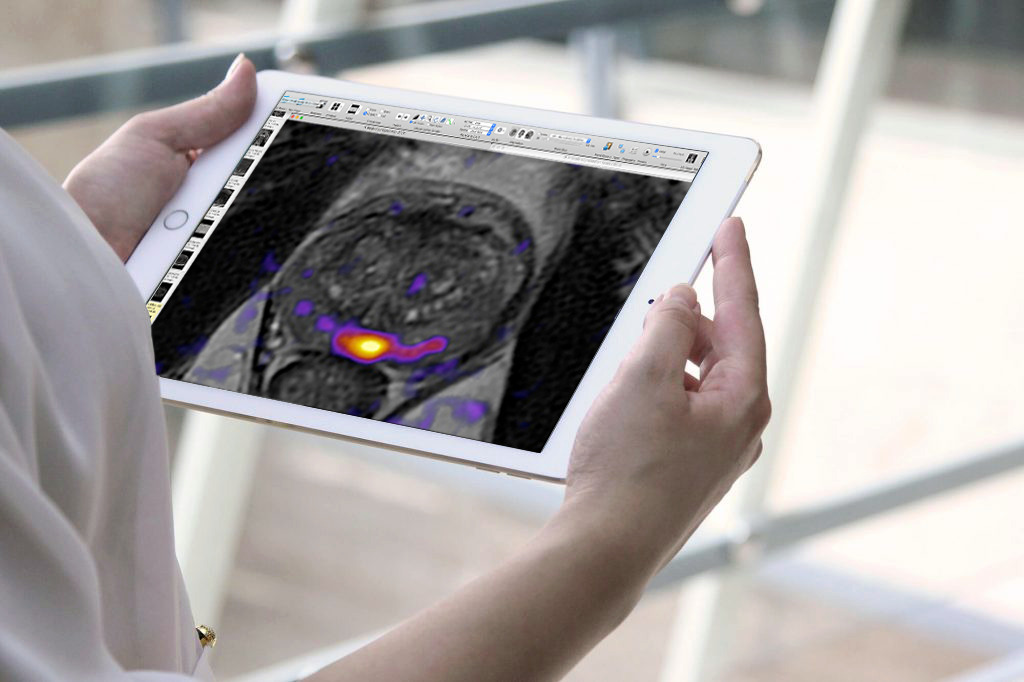
BlueLaser™ 3T mpMRI: Better Early Detection
If a high PSA raises suspicion of cancer, the next step before biopsy is to obtain an accurate 3D image of the gland that defines both normal and cancerous tissue. It is just as important to see what is healthy as what is unhealthy! Ultrasound doesn’t do this because it can’t reveal specific differences needed to detect what is and isn’t cancer.
Our BlueLaser™ 3T mpMRI Plus features the latest advance in multiparametric imaging sequences. It is called Restricted Spectrum Imaging (RSI) powered by AI, and it takes cancer detection to a whole new level. RSI was originally developed for brain imaging where it accurately picks up previously undetectable but telltale differences in neurological diseases. When applied to prostate imaging, potentially cancerous lesions literally stand out.
Studies now show that combining technological breakthroughs and expertise1 makes an essential difference. By offering the increased accuracy of both RSI2 powered by AI3 together with the pioneering experience of Dr. Sperling and his team, the Sperling Prostate Center remains at the forefront of prostate cancer imaging.
RSI-MRI+ leverages an advanced diffusion MRI technique called Restriction Spectrum Imaging, powered by AI, to enable faster, more accurate prostate cancer detection.
If BlueLaser™ 3T mpMRI rules out cancer, it gives peace of mind and avoids a biopsy or other additional testing. If, however, a suspicious area is detected and a biopsy is necessary, we offer the superiority of in-bore MRI-guided targeted biopsy.
Remember: Early prostate cancer has NO SYMPTOMS. Early detection results in better diagnosis, better treatment decisions and better outcomes.
MRI-Guided Targeted Biopsy: Better Diagnosis
A real-time prostate biopsy done in the bore (tunnel) of our powerful 3T magnet excels over all other biopsy methods.4 Standard 12-14 needle TRUS biopsies miss 30-40% of tumors. They over-detect insignificant prostate cancer (may not require immediate treatment) and under-detect significant prostate cancer (requires immediate treatment).
In-bore biopsy with fewer needles is twice as accurate as TRUS biopsy.5, 6 Patients are often told that a fusion biopsy is an “MRI-guided biopsy” but this is misleading. In fact, fusion is software that relies on previous MRI images overlaid on real-time ultrasound—an image manipulation process with technical pitfalls that can compromise imaging accuracy.7 Compare TRUS, fusion, and real-time in-bore MRI biopsies here.
Is BlueLaser™ 3T mpMRI Right for You?
“Knowledge is power only if man knows what facts not to bother with.” -R.S. Lynd
Our BlueLaser™ 3T mpMRI empowers our patients by providing accurate knowledge about what’s going on in their bodies, both normal and disease. You should consider BlueLaser™ 3T mpMRI for the earliest possible detection if:
- You have an elevated or rising PSA
- You have an abnormal DRE
- You were treated for a prostate infection or inflammation but your PSA is still high
- You are on Active Surveillance
- You are in a high-risk category to develop prostate cancer (genetic or environmental factors)
- You have not had a PSA test but you have unusual urinary symptoms
PSA: What’s Normal, and What Does it Mean?
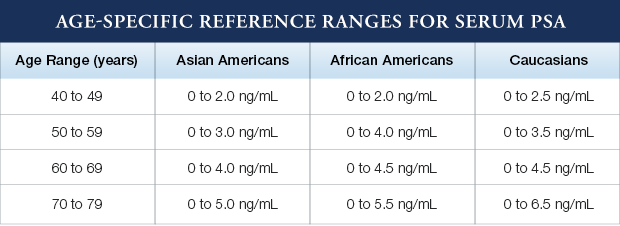
A higher-than-normal PSA can indicate noncancerous conditions such as aging-related enlargement, inflammation, or infection. Certain activities, such as riding a bike or having sex can trigger a temporary increase in PSA that has nothing to do with disease.
On the other hand, up to 15% of men with normal PSA levels can still have prostate cancer.8 Even when PSA levels are abnormal, as many as 75% of men end up not having prostate cancer yet have had unnecessary biopsies and worried for nothing.9
Also, the Digital Rectal Exam (DRE) is not reliable for detecting prostate cancer. The doctor can only feel the surface of the gland closest to the rectal wall, completely missing small tumors located more deeply where most prostate cancer begins. It is neither thorough nor accurate.10
Since the likelihood of having prostate cancer increases proportionately with PSA level, there is no threshold below which a man can be reassured that prostate cancer does not exist. PSA levels greater than 4 ng/mL are generally considered suspicious. As levels increase above 10.0 ng/mL, the probability of cancer increases dramatically. However, not all men with prostate cancer have elevated PSA levels, and not all normal PSA levels guarantee that no cancer is present. A small percentage (thought to be less than 15%) of prostate cancers can present with a PSA level of less than 4.0 ng/mL. This is why doctors may use lower thresholds to decide when to do a biopsy.
Excellence in Prostate Cancer Detection
The Sperling Prostate Center is a technologically-advanced, patient-oriented practice dedicated to providing the most effective techniques in prostate cancer detection and diagnosis. Unlike the PSA blood test or DRE, our approach—utilizing BlueLaser™ 3T mpMRI imaging with the newest advances in Restricted Spectrum Imaging, powered Artificial Intelligence—offers the best pathway to diagnostic superiority.
Take the next step today
Request your free consultation with Dr. Sperling, and we’ll work together to make the best diagnostic and treatment plan for you.
NOTE: This content is solely for purposes of information and does not substitute for diagnostic or medical advice. Talk to your doctor if you have health concerns or questions of a personal medical nature.
1 Pedler K, Kitzing YX, Varol C, Arianayagam M. The current status of MRI in prostate cancer. Aust Fam Physician. 2015 Apr;44(4):225-30.
2 McCammack KC, Schenker-Ahmed NM, White NS, Best SR et al. Restriction spectrum imaging improves MRI-based prostate cancer detection. Abdom Radiol (NY). 2016 May; 41(5): 946–953.
3 Bardis MD, Houshyar R, Chang PD, Ushinsky A et al. Applications of Artificial Intelligence to Prostate Multiparametric MRI (mpMRI): Current and Emerging Trends. Cancers (Basel). 2020 May; 12(5): 1204.
4 Wegelin O, van Melick HHE, Hooft L et a. Comparing Three Different Techniques for Magnetic Resonance Imaging-targeted Prostate Biopsies: A Systematic Review of In-bore versus Magnetic Resonance Imaging-transrectal
5 Kaufmann S, Kruck S, Kramer U, Gatidis S et al. Direct comparison of targeted MRI-guided biopsy with systematic transrectal ultrasound-guided biopsy in patients with previous negative prostate biopsies. Urol Int. 2015;94(3):319-25.
6 Wegelin et al., ibid.
7 Tay K.J., Gupta R.T., Rastinehad A.R., Tsivian E., Freedland S.J., Moul J.W., Polascik T.J. Navigating MRI-TRUS fusion biopsy: Optimizing the process and avoiding technical pitfalls. Expert Rev. Anticancer Ther. 2016;16:303–311.
8 Thompson IM, Pauler DK, Goodman PJ, Tangen CM et al. Prevalence of prostate cancer among men with a prostate-specific antigen level < or =4.0 ng per milliliter. N Engl J Med. 2004 May 27;350(22):2239-46.
9 Catalona WJ, Smith DS, Ratliff TL et al. Measurement of prostate-specific antigen in serum as a screening test for prostate cancer. N Engl J Med. 1991;324:1156-1161.
10 Totaro A. Is digital rectal examination still useful in prostate cancer diagnosis? NO! Urologia. 2019 Feb;86(1):32-33.